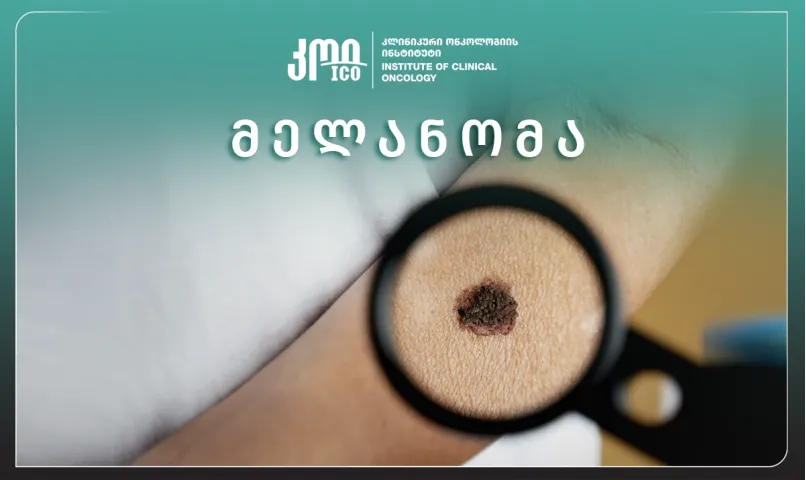
Are you interested in what kind of disease melanoma is? What are the statistics? Who is at high risk, how is it diagnosed, and treated? Is there any prevention, and why is monitoring important? Natia Mamadashvili, a doctor-oncologist at the Institute of Clinical Oncology, discusses this topic with us.
- What is Melanoma?
Melanoma of the skin is a malignant tumor that develops from melanocytes. Melanoma accounts for approximately 5% of all malignant skin tumors and is most common in white people living in sunny countries.
- What are the statistics?
Melanoma accounts for 5% of skin cancers, and the number of cases is increasing every year. The highest prevalence is in Australia and New Zealand. In young age, it is more common in women, but in old age in men.
- What are the causes?
The main factors are UV radiation, light skin type, and genetic predisposition.
All known etiological factors of skin melanoma are divided into exogenous and endogenous.
Exogenous factors: Ultraviolet radiation (UV): Prolonged and intense exposure to the sun, especially sunburns in childhood, increases the risk of melanoma.
Periodic, intense UV radiation (“holiday sun damage”) is particularly risky. Tanning beds: Frequent use of artificial UV radiation significantly increases the risk of developing melanoma. Geographical location and environmental conditions.
The intensity of solar radiation increases near the equator and in high-altitude areas.
People residing in sunny regions (e.g., Australia, South Africa) are at higher risk of melanoma.
- Is it possible for a medication or cosmetic to be a trigger?
Certain medications or cosmetics that cause a toxic reaction when exposed to the sun increase the risk of skin damage.
- Who is at highest risk?
Workers in chemical enterprises are at increased risk due to prolonged exposure to toxic substances. Inadequate UV protection (minimal clothing or lack of protective equipment) increases the risk. Incorrect use of sunscreen: improperly applied creams (e.g., only low SPF or at the wrong time of day). Outdoor working conditions that are exposed to strong sunlight (e.g., gardening, fishing). Air pollution and ozone layer depletion increase the intensity of UV radiation.
- Does genetic background matter?
If melanoma occurs in close family members, the risk increases significantly. Mutations in the CDKN2A (p16) and CDK4 genes are often associated with the development of melanoma.
MITF and BRAF mutations are associated with impaired melanocyte function.
- Does skin type matter?
Skin prone to fast sunburn (types I and II according to the Fitzpatrick classification). Fair skin color, blond or red hair, blue or green eyes. Number and quality of moles: Many normal moles (>50). Dysplastic (atypical) moles. General pigmentation: Albinism or hypomelanosis increases the risk of UV damage. Immunosuppressive conditions (e.g., after organ transplantation). Comorbid diseases that weaken the defensive ability of the body (e.g., AIDS).
- At what age is it most common?
Melanoma is more common in adults, although it can also occur in young people (especially between the ages of 25 and 50).
- Is it more common in women or men?
In young age, it is more common in women, but in elderly age in men.
- What is the importance of hormonal factors?
Pregnancy, menopause, and hormone therapy have a negative impact on the development of melanoma.
- What is the clinical picture?
There are 3 main types of melanoma: Superficial melanoma: The most common form (70-75%). It develops from a nevus and is characterized by long-term growth (over several years) with subsequent rapid transformation. It is more common in middle-aged people. Location - on the back in men, on the shins in women. The tumor has small dimensions, irregular shape and edges. Brown and dark brown melanomas with slight bluish inclusions are more common. Both vertical and horizontal growth of the tumor is possible. Such melanomas have a tendency to ulcerate and bleed. The prognosis is usually favorable. Nodular melanoma occurs in 15-30% and is a more aggressive form. It occurs mostly in older people. This type of melanoma grows rapidly (vertically). About 5% of nodular melanomas do not have pigment. The prognosis is unfavorable.
Lentigo-melanoma (melanoma freckle, malignant lentigo) occurs in 4-10% of cases. It develops over the age of 70. Nodules appear on the skin in the form of dark blue, dark brown or light brown spots. With a diameter of 1.5-3 mm. The face, neck and other open areas of the body are more often affected. These melanomas can develop from melanotic freckles. The prognosis is favorable. Subungual melanomas can occur under the mask of paronychia, purulent lesions of the fingers. Melanomas of the mucous membranes: can be of different colors or colorless. Localized in the conjunctiva, oral or nasal cavity, vaginal or rectal mucosa. Skin melanomas are of different sizes, shapes, surfaces, consistency and color. The tumor can be small, in the early stages the diameter of the tumor does not exceed 1-2 cm, in the late stages it can be large.
- How do the tumorous nodes develop?
Melanoma can be manifested as a flat pigmented spot, having a mushroom shape. It can be on a leg or a wide bottom. Its surface can be smooth, even shiny, mirror-like. Later, small ulcers appear, and bleeding can occur with even a minor trauma.
- What are the earliest and most unfavorable signs of malignancy?
- Nevus growth on the surface
- Asimetric edges
- Nevus surface desquamation (shedding)
- Color changing
- Itching and burning
- “ABCD”- rule of malignancy:
- A – Asymmetry
- B – Border (irregular shape of borders)
- C – Color (darker than other formations with inclusions of different colors)
- D – Diameter (size >6mm)
- How is the stage determined?
0 Stage (In Situ) The tumor is confined only to the epidermis (outer layer of the skin). There is no metastasis. Prognosis: 100% cure with early intervention.
I stage (early invasive melanoma) the tumor thickness: IA: ≤1 mm melanoma without ulceration. IB: 1-2 mm melanoma, or ≤1 mm with ulceration. There is no metastasis. Prognosis: Very high chance of cure
II stage (localized melanoma) tumor thickness: IIA: 1-2 mm with ulceration or 2-4 mm without ulceration.
IIB: 2-4 mm with ulceration or >4 mm without ulceration. IIC: >4 mm with ulceration. Lymph nodes and metastases are not affected. Prognosis: Depends on tumor tikness and presence of ulceration.
III stage (regional melanoma) The tumor has spread to nearby lymph nodes or to nearby skin. Ulcers are often present. Prognosis: Varies depending on the stage; treatment often includes surgery, immunotherapy, or targeted therapy.
IV stage (metastatic melanoma) The tumor is spread to distant organs (e.g., lungs, liver, brain) or to distant skin. Symptoms: General weakness, weight loss, organ dysfunction due to metastases. Prognosis: Depends on the location of the metastases and the body's response to treatment. The following features of melanoma have the greatest diagnostic value:
- Disappearance of the skin pattern on the surface of the nevus
- Formation of a shiny, glossy surface of the nevus
- Horizontal growth of the nevus
- Ulceration of the epidermis over the nevus
- Wetting, bleeding of the surface of the nevus
Diagnostics:
History: Changes in mole size, color, or shape.
Itching, bleeding, or painful mole.
Family history of melanoma or skin cancer.
ABCDE criteria (basic method for assessing moles)
- How is the diagnosis made?
Dermatoscopy allows for the assessment of the mole microscopically. The doctor evaluates the structure, color, borders, and vascular changes of the pigmented spots. If the mole or spot is suspicious, a skin biopsy is performed. Incisional or excisional biopsy: Complete or partial removal of the affected area. Histological examination of the biopsy specimen is the gold standard for confirming melanoma. Laboratory and immunohistochemical studies S-100, HMB-45, and Melan-A: Markers used in the diagnosis of melanoma. BRAF mutation test: Used to identify genetic mutations, which are important for choosing a treatment method.
- What is the treatment?
Treatment for local lesions: Local excision: Extensive excision of the primary tissue within borders of healthy tissue is necessary. Routine selective lymphadenectomy is not recommended. Treatment for local-regional lesions: All patients with regional lymph node involvement are treated with:
- Radical lymphadenectomy
- Immunotherapy
- Targeted therapy
- Chemotherapy
- Radiation therapy
- Adjuvant and nonadjuvant therapy
- Experimental methods
- Monitoring and follow-up care
- Is monitoring needed?
Monitoring is recommended every 3 months for the first 2 years and then every 6-12 months.
- Is there any prevention?
It is necessary to identify individuals at increased risk of developing skin cancer and melanoma, for whom the recommendations are:
- Limiting sun exposure
- Using sunscreen
- Protecting pigment spots from trauma
- Removing nevi in areas at risk of trauma (when touched by clothing or shoes) Monitoring nevi that are on the soles of the feet, ankles, and nail beds.
- Views:2109