Tumor immunotherapy – a new paradigm in lung cancer treatment
Lung cancer is the most common tumor throughout the world. Annually, the mortality rate (1 590 000) caused by this disease equals the summed indicator of mortality caused by colon, prostate, and breast cancer.
Based on the structure of the tumor tissue, lung cancer is divided into two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
Non-small cell lung cancer (NSCLC) is more common and accounts for 80% of cases, while small cell lung cancer (SCLC) accounts for 20%. Most cases are advanced forms of the disease.
On August 13, the prestigious medical journal The New England Journal of Medicine (NEJM) published an article titled “Effect of the Latest Achievements in Lung Cancer Treatment on Population Mortality”. It states that for the first time in several years, mortality caused by lung cancer has started decreasing.2
Naturally, the question has been raised: "what led to such a transformation in lung cancer treatment?
By using modern methods of diagnosing and treating lung cancer it is possible not only to study the tissue structure of the tumor, but also to perform an in-depth study of its molecular biomarkers, and develop so-called precision treatment tailored to them. Lung cancer tissue is rich in such biomarkers and most known from them are EGFR (epidermal growth factor receptor), ALK (anaplastic lymphoma kinase), PD-L1(programmed death ligand 1), ROS (receptor tyrosine kinase), and also other markers. They can be detected through the in-depth, comprehensive, molecular diagnostics of lung cancer biopsy material that serves as a base for the selection of targeted treatment.
It’s namely the application of targeted treatment and tumor immunotherapy in clinical practice that has greatly contributed to reducing the mortality rate caused by the disease.
Let’s briefly look at tumor immunotherapy – what it means, how the immune system fights cancer, and what type of treatment it involves.
The application of the immune system to fight cancer is actually “a new version of an old fairy tale”. 1890s, New York-based surgeon William Coley started injecting patients with bacteria to treat cancer. “Coli toxins,” as they are now called, provide one of the first pieces of evidence that immune system stimulation leads to shrinking or elimination of tumorous growths.
In recent periods, modern anti-tumor treatment approaches mostly focus on gene mutations, causing abnormal tumor development. 3
The real change occurred when immune system suppressors, so-called “checkpoint inhibitors,” were discovered on the surface of tumors. These include: PD-1, PD-L1, and CTLA-4, which suppress the activity of the main cells of the immune system - T lymphocytes.
These biomarkers are also moderately expressed on normal cells (including immune cells). They prevent the self-activation of the immune system and the development of autoimmune processes. In the case of tumor formation, the over-expression of checkpoint markers inhibits the activity of immune cells, and as a result, the immune system deactivates.
Nowadays, the following types of tumor immunotherapy drugs are known - the so-called "checkpoint" inhibitors: anti-CTLA-4, anti-PD1, and anti-PD-L1. Their action mechanism involves disrupting the connection between the inhibitory marker of the tumor cell and the immune cell and destroying the tumor cell by reactivating the immune cells.
The stated article notes that recent immunotherapy-based therapies-specifically, programmed death ligand 1 (PD-1, PD-L1) inhibitors - have significantly improved the outcome of non-small cell lung cancer. In randomized, phase 3 trials, these drugs have shown an increase in median survival compared to standard chemotherapy.2
These treatment strategies can be used both as monotherapy or as combined treatment - with chemotherapy, targeted therapy, or immunotherapy.
Tumor immunotherapy drugs are used in both first- and second-line lung cancer treatment in previously treated patients.
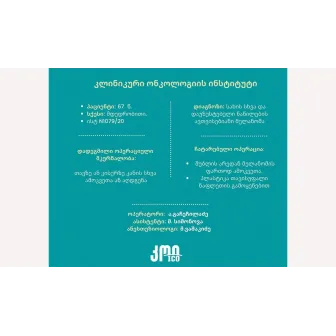
It is gratifying that Georgian oncologists also have quite extensive and rich clinical experience in the application of tumor immunotherapy for lung cancer, both within the framework of clinical trials and independent clinical practice.
Also, an anti-PD-L1 group tumor immunotherapy drug has been registered in Georgia for several years.
1. Ferlay J, et al., GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide [document on the Internet]. International Agency for Research on Cancer; 2013 [cited 2016 Nov 21]
2. N Engl J Med 2020;383:640-9. DOI: 10.1056/NEJMoa1916623
3. Cancer Research UK. What is Coley’s toxins treatment for cancer?
- Views:2791